The pros and cons of 8 different birth control methods

Luckily for us now, safe and proven methods of birth control – from injections, pills, to even an app – are readily available. But even so, gynaecologists tell us that contraceptive myths and misconceptions still exist today, albeit a lot less bizarre than crocodile poo.
“There is a general ignorance and misconception about the use of contraceptives in Singapore,” says obstetrician and gynaecologist Christopher Ng, medical director of GynaeMD Women’s and Rejuvenation Clinic.
“For instance, the pill is underused here even though it is actually more effective (in preventing pregnancy) than condoms. Many women shy away from using oral contraceptives because they have misconceptions about how taking hormones is bad for them, or that it can lead to infertility later on,” he adds.
A multinational survey commissioned by pharmaceutical giant Bayer Schering Pharma has found that Singapore women are particularly confused about contraceptive options, compared to women in other regions.
More than half of the young Singaporean women – 60 per cent – surveyed admitted they were not very familiar with the various birth control options available.
About one in five and over a third also thought that sex during menstruation and the withdrawal method are effective forms of contraception, even though gynaecologists say these methods are actually highly unreliable.
And then there are some women who still believe that emptying the bladder and bathing after sex can prevent pregnancy – totally unscientific, unfortunately.
In Singapore, the male condom remains one of the most popular contraceptive options, experts say.
On the contrary, other forms of barrier methods such as the female condom, diaphragm and cervical cap lag far behind in popularity and effectiveness because “women tend to be uncomfortable about having to put them on”, says Dr Wee Horng Yen, obstetrician and gynaecologist at The O&G Care Clinic.
In spite of the popularity of the male condom, Dr Christopher Chong, obstetrician, gynaecologist and urogynaecologist of Chris Chong Clinic, says many couples end up using them incorrectly. This barrier method is up to 98 per cent effective in preventing pregnancy, but the figure drops drastically when used incorrectly.
To be safe, there should be no direct contact between the penis and the vagina before the condom is worn. “This is because pre-ejaculation secretions may have even more sperm count than in the actual ejaculation itself,” explains Dr Chong. He adds that it is also important to “squeeze the air pocket at the tip of the condom” before putting it on to prevent tearing. “People think all they need to do is to put it on and that’s it, but a condom is only effective if it’s worn correctly,” says Dr Chong.
The doctors interviewed all stress that there is no one-size-fits-all contraceptive method.“What suits you will depend on your age and lifestyle,” says Dr Ng.
Before settling on any option, the experts suggest doing your own research and speaking with your doctor to figure out which contraceptive will work best for you.
To help you along,we take a look at various contraceptive options available.

What:Taken daily, the combined oestrogen and progestogen pill prevents ovulation.
How effective:Up to 99 per cent if used correctly.
The good: The pill is one of the most effective forms of birth control. Your fertility returns immediately when you stop taking it. Plus, there are other non-contraceptive benefits, too.
Dr Wee cites a lower risk of ovarian and endometrial cancer. It also helps regulate the menstrual cycle, manage acne and improve PMS symptoms.
The bad: For those who hate popping pills, this can be a hassle as you have to remember to take it every day for it to work properly. It is also unsuitable for certain women, such as those with health problems, or are on certain medications.

What: A thin patch that works in the same manner as the pill. It is worn anywhere on the abdomen, thigh, buttocks or arm and changed weekly.
How effective: Up to 99 per cent if used correctly.
The good: Dr Chong says the patch is a good alternative for people who find pill-popping a hassle. Users also experience “fewer gastric effects” than those on the pill.
The bad: The patch is not transparent. Plus, Dr Ng says it can get a tad annoying and uncomfortable, no thanks to Singapore’s hot and humid weather. “There’s also a psychological effect – some women get insecure because they are not sure if it will fall off,” Dr Ng adds.

What: A shot in the buttocks or arm to prevent ovulation.
How effective: Up to 99 per cent.
The good: If you find popping pills or changing patches way too troublesome, consider this. You only have to do this once every three months. This is also suitable for breastfeeding mums, says Dr Wee. Other pros include light or possibly no periods after a year.
The bad: Weight gain and irregular bleeding in the first three months are common side effects. You may also end up forgetting to take your shots. Dr Ng adds that you may also have to wait six to 12 months to regain your fertility after you stop the injections.

What:This smartphone fertility tracking app is the first in the world to be government-approved as a contraceptive, putting it alongside the pill, coils and condoms – in Europe, at least.
How effective: A clinical study has proven that using the app is as effective as a method of birth control as being on the pill.
The good: There are no side effects since no medication is involved. To use the app, women measure the temperature underneath their tongues every morning and enter the measurement into the app.
An algorithm developed uniquely for the app then determines whether you’re fertile or not that day, so you know if you risk pregnancy by having unprotected sex.
The bad: Because it is a fertility-based awareness method of contraception, critics say it isn’t always reliable, because our bodies could be affected by various factors, including stress.

What:Inserted under the arm to prevent ovulation, this progesterone implant slowly releases hormones to prevent pregnancy.
How effective: Up to 99 per cent.
The good: The implant, which lasts for three years, is good if you’re looking for a long-term contraceptive option. You will also regain your fertility quickly after you stop using it.
The bad: Weight gain, irregular menses and bloating are some common side effects you may experience. You will need to see a doctor to get it inserted. In rare instances, removing the implant may be a challenge if it is too deeply embedded, says Dr Chong.

What: Also called the coil, this is a small T-shaped copper device which is inserted into the uterus to prevent pregnancy.
How effective: Up to 98 per cent.
The good: The coil can be left in the womb for up to five years. Your fertility resumes immediately once you remove it.
The bad: It may cause irregular bleeding or spotting. Doctors don’t usually recommend this as a first choice for anaemic women or those who have heavy periods.
In rare instances, there is a small risk that the IUD may fall out and cause an infection during the insertion, Dr Wee says. Other risks include difficulty in removing the device.

What: This small plastic device, which is inserted into the uterus, works like the coil, except that it has an added hormonal (progestogen) effect.
How effective: It works almost like permanent sterilisation, and is more than 99 per cent effective, Dr Wee says.
The good: The mirena can stay in place for about five years, and fertility resumes once you remove it. Besides its contraceptive effects, the device also has other benefits.
Dr Wee says it helps reduce heavy periods, painful menstrual cramps and symptoms of adenomyosis, a painful gynaecological condition. About one in five women who have been on the mirena for six months will have no periods or have only light staining.
The bad: You may bleed a lot in the first three months, warns Dr Chong. The Mirena carries similar risks as the IUD.
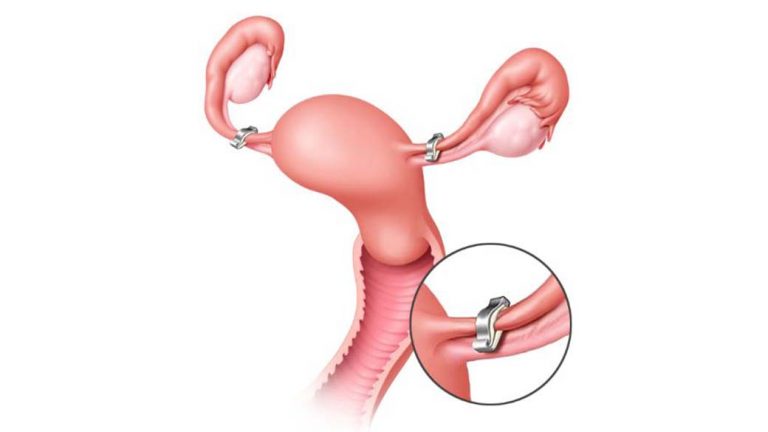
What form of contraception where the fallopian tubes – which carry eggs from the ovaries to the womb – are surgically cut.
How effective: More than 99 per cent effective.
The good: Sterilisation is a good option for women who are certain that they no longer want more children.
The bad: Most doctors do not recommend this procedure. After all, with so many other forms of non-permanent forms of contraception available, why opt for something that is almost irreversible?
This article was first published in Young Parents.